Multidisciplinary research at Sylvester Comprehensive Cancer Center, fueled by a five-year, $2.9 million National Cancer Institute grant, is designed to test the benefit of a novel quantitative MRI imaging algorithm developed at the University of Miami, in combination with blood biomarkers, in selecting patients who should or should not have a prostate biopsy.
Principal investigators Alan Pollack, M.D., Ph.D., professor and chair of radiation oncology and interim deputy director of Sylvester Comprehensive Cancer Center; Radka Stoyanova, Ph.D., professor and director of imaging and biomarkers, radiation oncology; and Sanoj Punnen, M.D., a urologic oncologist at Sylvester and associate professor of urology at the Miller School of Medicine, are collaborating for the single-site study, doing what Dr. Punnen calls “team science.”
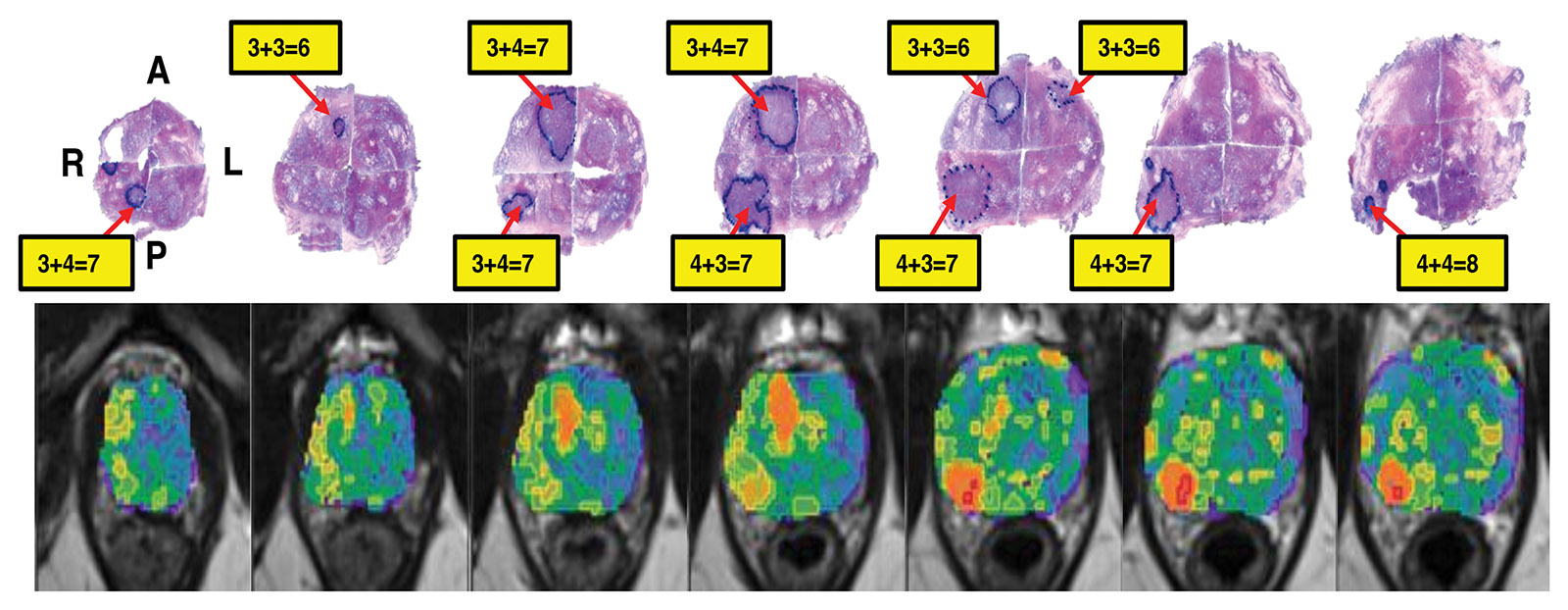
Together, they are studying undiagnosed men using quantitative multiparametric MRI to determine if the technology developed by the group, when combined with blood biomarkers, improves the selection of patients who are at a very low risk of having a significant prostate cancer. “Our team has run several clinical trials that provided a framework for the development of software that automates the identification and risk classification of areas in the prostate that should be biopsied,” Dr. Pollack said. Current methods for deciding where to place a needle in the prostate for sampling are much more subjective. “Our approach takes the guesswork out of needle placement for sampling.”
Multiparametric MRI is rapidly becoming the cornerstone for whether to biopsy and where in the prostate to biopsy. The technology is evolving and Sylvester is at the forefront of these advances.
“If the MRI is positive, it suggests the man needs a biopsy. It can also help guide where you put the needle,” Dr. Punnen said. “If the MRI is negative, the downside is there’s still a 10% to 30% chance there could be a cancer that we just didn’t see on the MRI.”
The need for better detection and a series of studies and discoveries at Sylvester formed the basis of this latest grant, Dr. Punnen said. Dr. Stoyanova’s group built an image-analysis algorithm and found it did a better job of picking out significant prostate cancers than the standard of care system for scoring prostate MRI.
“We are now testing our scoring system, termed the habitat risk score, along with more sophisticated deep learning methods, for more accurate detection of significant prostate cancer and the decision of whether there is a need for biopsies,” Dr. Stoyanova said.
In this study, the researchers will look at a collection of blood markers. They hypothesize that the 30% potential uncertainty with the current standard-of-care MRI at most academic institutions could fall to 16% uncertainty with the artificial intelligence (AI) algorithm. Adding blood markers could bring the level of certainty to more than 90% and uncertainty to less than 10%, according to Dr. Punnen.