The cornerstone of CABC is the Transitional Bereavement Care Model. This model promotes continuity of care for the patient’s chosen family through bereavement. It also calls attention to the responsibility that health systems have to help grievers transition from institution-based bereavement resources to care in the community, advocating for the use of evidence-based assessments and support in both settings. CABC is founded on the belief that building up support in the community and this type of transitional care can address the gap between the naturally finite resources offered by health-systems and more sustainable care available within the community.
Below are additional resources describing the Transitional Bereavement Care Model and how it informs our work at the Center for the Advancement of Bereavement Care.
To hear more about this model from a public health viewpoint, please find The Lancet publication here:
https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(24)00030-6/fulltext
To hear more about this model and how it informs our work at Sylvester Comprehensive Cancer Center, please find our publication with University of Miami Miller School of Medicine News here:
https://news.med.miami.edu/sylvester-calls-for-bereavement-funding/
To see a visualization of the model and recommended components of institutional and community supports, see below:
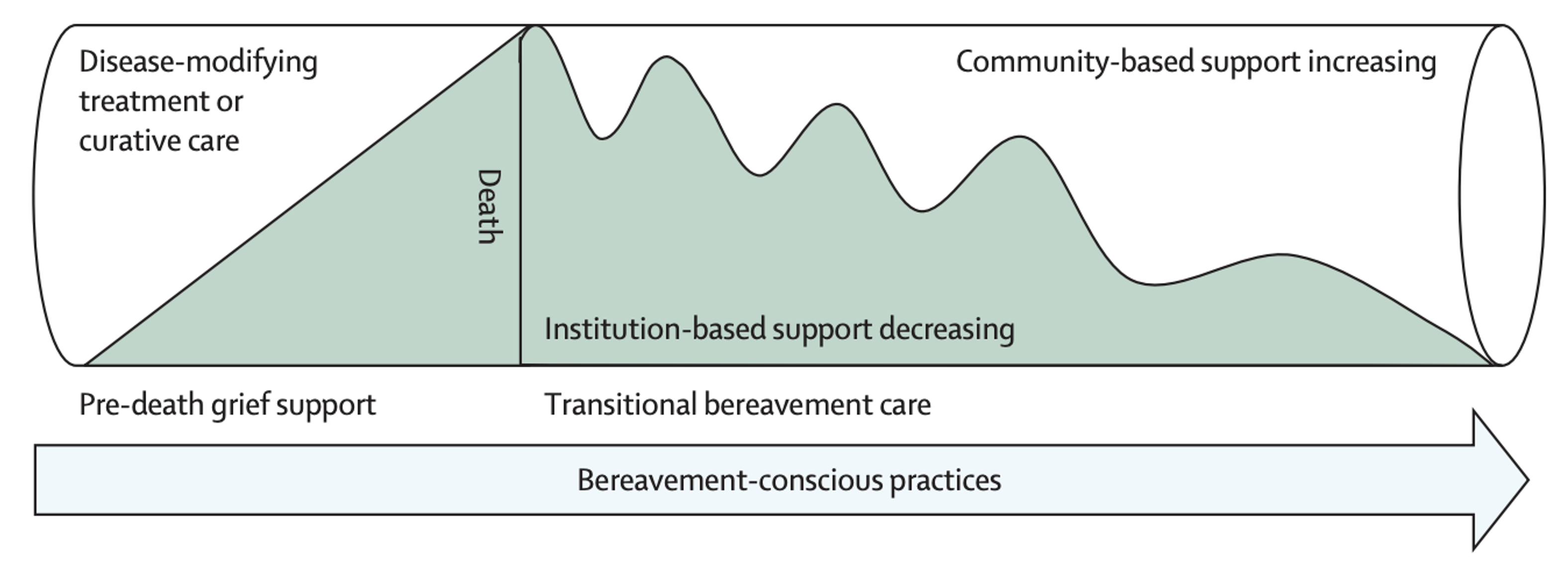 Figure: Conceptualising transitional bereavement care. From “Investing in bereavement care as a public health priority,” by W.G. Lichtenthal, K.E. Roberts, L.A. Donovan, L.J. Breen, S.M. Aoun, S.R. Connor, W.E. Rosa, 2024, April 1, The Lancet Public Health, 9(4), pp.e270-e274.
Figure: Conceptualising transitional bereavement care. From “Investing in bereavement care as a public health priority,” by W.G. Lichtenthal, K.E. Roberts, L.A. Donovan, L.J. Breen, S.M. Aoun, S.R. Connor, W.E. Rosa, 2024, April 1, The Lancet Public Health, 9(4), pp.e270-e274.
| Establishment of institutional supports | Development of community supports | |
|---|---|---|
| Preventive bereavement care | Health-care teams engage in bereavement-conscious practices, mindful of pre-death grief and the potential effect of end-of-life experiences on the bereaved family and of the importance of their relationships with the family of the dying patient. | Compassionate communities are mindful of the emotional and practical needs of the family of the dying patient. |
| Ownership of bereavement care | Institutions provide bereavement services and have dedicated personnel to educate clinicians and staff, conduct bereavement risk screening, reach out to bereaved individuals, develop bereavement resources, and provide counselling or grief support. | Bereavement care centres are sustained in the community and bereavement care champions are identified for universal bereavement care within relevant organizations (eg, workplace, schools, religious institutions, or care facilities for older people) |
| Resource allocation for bereavement care | Resources, including dedicated, funded personnel, are allocated to offer universal outreach and resources for all bereaved individuals (eg, condolence calls, memorial services, educational and web-based resources, and peer to peer and group support) and to provide targeted support to those in need. | Bereaved stakeholders provide input to institutions, communicate needs, and liaise with groups in the community to identify barriers and facilitators to bereavement support and to determine needed resources, integrating intersecting social identities (eg, religion, ethnicity, or class) |
| Upskilling of support providers | Bereavement care education is integrated into medical and health worker training programs; institutions provide continuing bereavement care education to all staff as well as dedicated bereavement specialists. | A workforce of trained bereavement specialists in the community who are accessible (eg, accept insurance); community education about how to compassionately support the bereaved and increase grief literacy. |
| Implementation of evidence-based care | Bereavement care is evidence based; research funding is available for the development of effective grief assessments, interventions, and training programs. | Research is designed and implemented in partnership with grievers and communities to co-create best practices to support the bereaved. |