New cutting-edge technology that uses artificial intelligence along with optical imaging is providing neurosurgeons a near real-time method of diagnosing brain tumors during surgery, according to a collaborative study co-authored by neurosurgeons with Sylvester Comprehensive Cancer Center, part of the University of Miami Miller School of Medicine, published in the journal Nature Medicine.
“It’s really a step forward in providing rapid intraoperative diagnoses of malignant and benign tumors, which is essential information needed to make critical decisions during safe and effective brain tumor surgery,” said Sylvester neurosurgeon and study co-author Michael Ivan, M.D., M.B.S., who played a major role in developing the Stimulated Raman Histology (SRH) technology with leading collaborators at New York University and the University of Michigan. “This digitized process provides surgical teams a diagnosis in less than three minutes as opposed to a 20-30 minute wait time during a traditional process.”
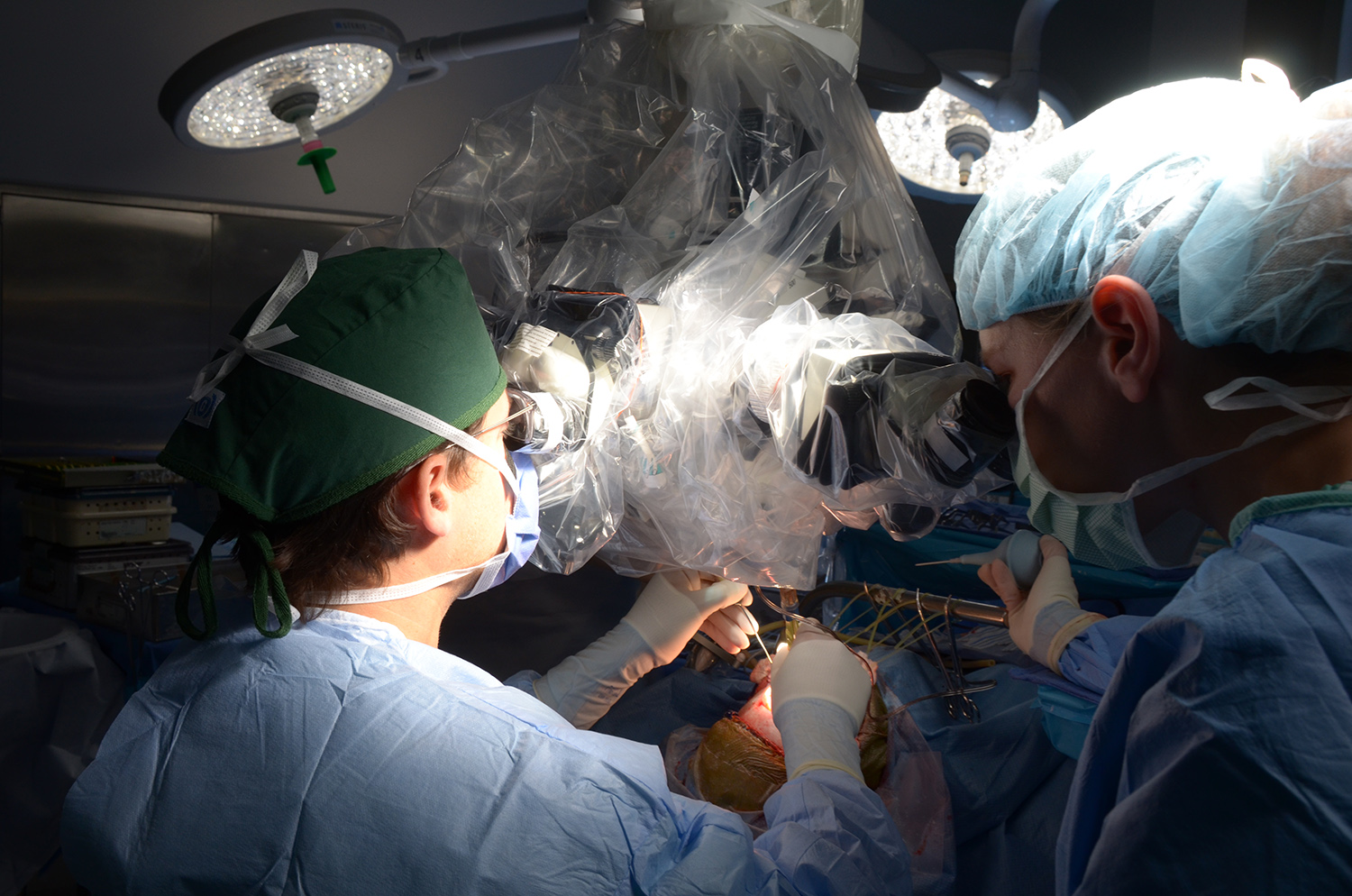
Accurate histopathologic diagnosis is crucial for planning during the actual surgical removal of brain tumors. Conventional methods for intraoperative histology are time consuming and require sectioning and freezing and necessitate tissue transport to a pathology laboratory, specimen processing, slide preparation by highly trained technicians, and interpretation by pathologists, with each step representing a potential barrier to delivering safe, timely, and effective surgical care.
Titled “Near Real-time Intraoperative Brain Tumor Diagnosis Using Stimulated Raman Histology and Deep Neural Networks,” the study examined the diagnostic accuracy of brain tumor image classification through machine learning, compared with the accuracy of conventional histologic images interpreted by pathologists. The results for both methods were comparable: the AI-based diagnosis was 94.6% accurate, compared with 93.9% for the pathologist-based interpretation on a frozen specimen.
One of the most significant advantages of Stimulated Raman Histology is ensuring more precision in completely removing cancerous brain tumors, said Dr. Ivan, who is leader of the Neuro-oncology Site Disease Group at Sylvester and assistant professor of neurological surgery at the Miller School of Medicine.
“In many of our surgeries on malignant tumors, the ability to remove all of the tumor makes a difference in a patient’s overall survival,” said Dr. Ivan. “Artificial intelligence provides more rapid and frequent information to the surgeon while operating to ensure the boundaries of the surgical resection are clear of cancer.”
This game-changing technology is an exciting step forward in the management of brain tumors, said Sylvester neurosurgeon Ricardo Komotar, M.D., who also served as a study co-author and is the director of surgical neuro-oncology and the Brain Tumor Initiative at Sylvester.
The pioneering imaging technique reveals tumor infiltration in human tissue by collecting scattered laser light that illuminates essential features not typically seen in standard histologic images.
The microscopic images are then processed and analyzed with artificial intelligence, and in under two and a half minutes, surgeons are able to see a predicted brain tumor diagnosis. Using the same technology, after the resection, they were able to accurately detect and remove otherwise undetectable tumors.
“This is a very complex AI system, which looks at patterns, intensity, and coloration of the specimen’s digital image to provide an instantaneous diagnosis,” said Dr. Ivan.